A research report from Japan sheds light on individual responses to dutasteride, a commonly used medication to treat benign prostatic hyperplasia (BPH), and also suggests that the drug helps to relieve urinary symptoms even in people who don’t show a significant reduction in prostate volume. The paper, “Effects of dutasteride on lower urinary tract symptoms: a prospective analysis based on changes in testosterone/dihydrotestosterone levels and total prostatic volume reduction,” appeared on Feb. 18, 2016, in the journal The Aging Male.
BPH — common in aging societies and marked by an enlarged prostate — can have troubling symptoms, but it is neither life-threatening nor causes cancer. Symptoms may include problems urinating, infection, reduced kidney function, or bladder stones.
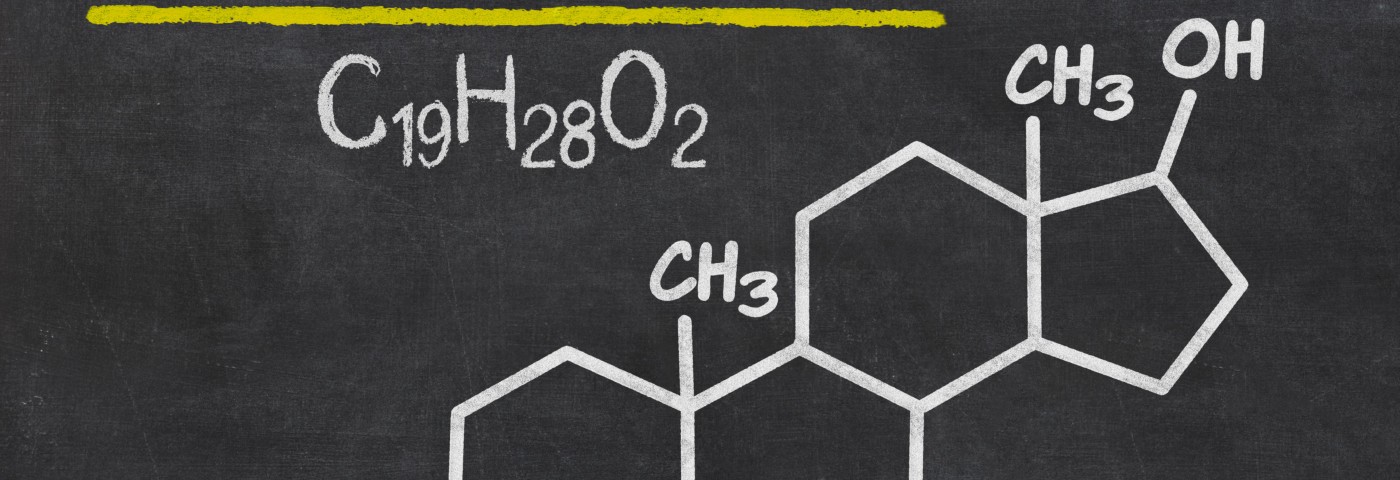
Dutasteride, also known as Avodart, is used to treat enlarged prostate caused by BPH. The medication works by inhibiting 5-alpha reductase, an enzyme that converts testosterone into dihydrotestosterone (DHT).
The analysis focused on the effects of dutasteride on lower urinary tract symptoms. Researchers, led by Kazuyoshi Shigehara of the 1 Department of Urology, Ishikawa Prefectural Central Hospital, in Kanazawa, assessed changes in total testosterone compared to DHT levels, and also gauged total reduction of the prostate, defined as total prostate volume (TPV). The scientists took measurements both before and after dutasteride treatment. Sixty men with BPH participated in the study, and took 0.5 mg of dutasteride each day for 52 weeks.
A total of 43 study subjects experienced reductions in TPV of 5 percent or more, and the remaining 17 had less than a 5 percent reduction. In the group with greater prostate reduction, higher level of DHT compared to total testosterone were reported. Both groups experienced improvements in symptoms including urinary problems, although improvements were more frequently noted in the group that experienced a 5 percent or greater TPV reduction.
The study demonstrated that baseline DHT and testosterone levels could predict the response to dutasteride, although benefits can still be observed in people with a low DHT to total testosterone level.
“Although TPV reduction induced by dutasteride treatment is likely to be dependent on individual 5-alpha reductase activity, effective benefits may not always depend solely on TPV reduction. Patients with less TPV reduction using dutasteride may also experience benefits in their voiding symptoms as a result of an increase in testosterone levels subsequent to undergoing this therapy,” the researchers concluded.
Dutasteride may help to improve urinary symptoms, the study found, even when prostate volume is not substantially reduced. The work also sheds light on possible biological markers for predicting who will best respond to this drug.