A study of the immunological involvement in the development and progression of benign prostate hyperplasia (BPH) looked at the correlation of the clinical parameters of the disease with the immune activation within the prostate.
The study, “Progression of benign prostatic hyperplasia is associated with pro-inflammatory mediators and chronic activation of prostate-infiltrating lymphocytes,” published in Oncotarget, suggests what has previously been suspected — that the progression of BPH is associated with pro-inflammatory mediators, and prostate-specific lymphocytes might be chronically activated.
BPH is a condition that leads to the non-malignant enlargement of the prostate gland and is associated with the onset of bladder outflow obstruction and a series of lower urinary tract symptoms (LUTS), all of which can greatly affect a patient’s quality of life. The pathogenesis, or development, of BPH is still not clearly understood, but general consensus points to a series of factors, such as changes in epithelial cell and stromal cell interactions and changes in the local endocrine system.
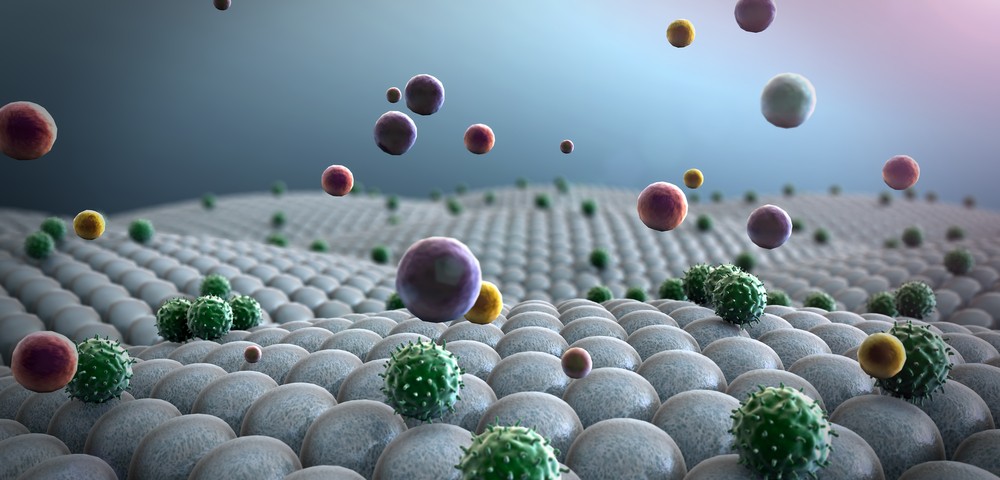
Increased infiltration of immune cells and pro-inflammatory factors have also been observed in BPH, but the concrete role of inflammation and immune cells in disease pathogenesis remains poorly defined.
Researchers compared the profiles of prostate-infiltrating lymphocytes (PILs), isolated from BPH tissues obtained from 31 patients, and their counterparts isolated from peripheral blood. Researchers also identified possible pro-inflammatory factors that might be involved in BPH lesions.
Results show indications of chronic activation of immune cells, supported by the increased number of T cells expressing co-inhibitory receptors (LAG-3, PD-1, TIM-3, and CTLA-4) in BPH tissue compared to peripheral blood. The results confirm the presence of abundant soluble pro-inflammatory factors in BPH-affected tissue, supporting previous studies that found pro-inflammatory cytokines and chemokines produced by BPH-derived cells.
Importantly, the size of the prostate and PSA levels correlated with different lymphocyte subsets and pro-inflammatory soluble molecules, suggesting a possible involvement in disease progression.
Researchers conclude that follow-up studies should look further at these results, and “detailed characterization of infiltrating immune cells and the microenvironment in healthy, BPH and malignant prostate tissue could help to develop new approaches to prophylactic and therapeutic treatment of prostate cancer.”