Bipolar “button” plasma vaporization of the prostate (BPVP) has better short-term results and is associated with fewer complications than classic transurethral resection of the prostate (TURP) in men with benign prostatic hyperplasia, according to recent findings.
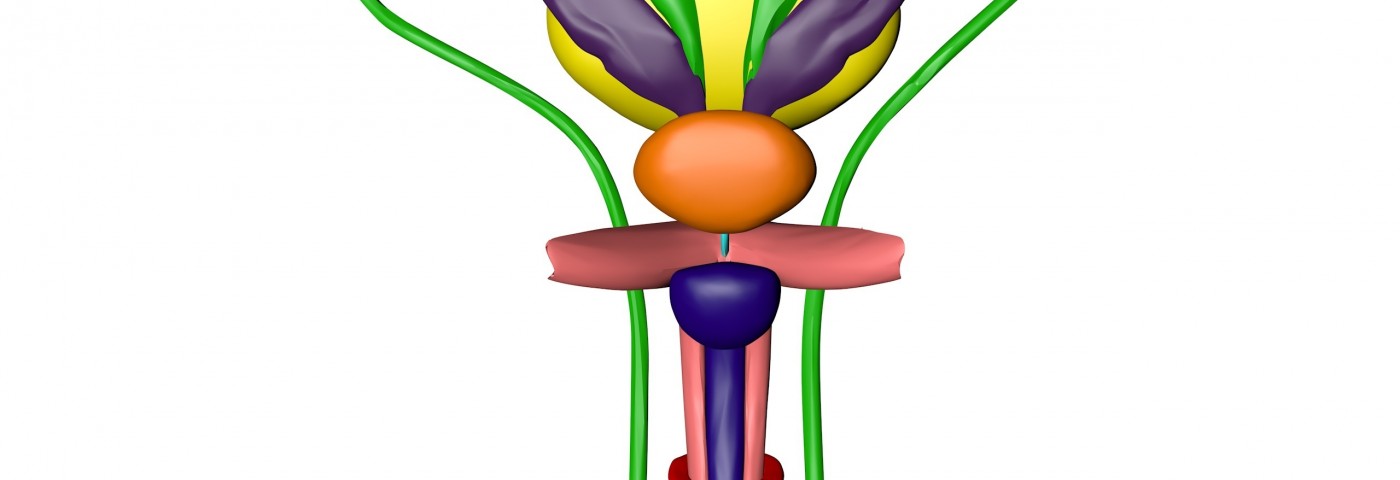
The BPVP technique resembles TURP, but uses isotonic saline for irrigation instead of glycine, and a button-type vaporization electrode.
The study – a collaborative effort between researchers from Minoufiya University Hospitals in Egypt and Mayo Hospital in Yemen – enrolled 152 patients with BPH. The group consisted of 100 men who underwent TURP and 52 who underwent the BPVP procedure.
The researchers evaluated men before surgery, and then 24 hours and three months post-surgery. The team measured a large number of parameters, including International Prostate Symptom Score, quality-of-life, urinary flow, and post-void residual urine.
According to the study, “Efficacy of bipolar “button” plasma vaporization of the prostate for benign prostatic obstruction, compared to the standard technique,” they also analyzed whether there were any differences in surgery, or hospital stay time, length of catheterization, blood loss, serum sodium levels, or presence of complications, between the groups.
Findings published in the journal Urology Annals show that patients in both groups had similar characteristics before the surgical procedure. Time of surgery and length of hospitalization was shorter for patients undergoing the BPVP procedure. The BPVP group also had the catheter for a shorter time and had less blood loss and serum sodium changes than patients undergoing TURP.
Two patients in the BPVP group experienced early complications, compared to 18 patients in the TURP group. No patients undergoing BPVP suffered substantial blood loss or developed TURP syndrome – a potentially life-threatening condition associated with the absorption of the glycin irrigation fluid used in TURP.
In the TURP group, two patients developed the syndrome, and six patients needed a blood transfusion after substantial blood loss. Two patients in the BPVP, and three in the TURP group, experienced narrowing of the urinary tube at the three-month follow-up.
After three months, BPVP patients reported lower symptom scores and better quality of life than men who had undergone TURP. They also had better urinary flow parameters.
The short-term results of the bipolar “button” plasma vaporization technique seem to be superior to TURP in both efficiency and safety. The authors noted that future trials, in addition to exploring the long-term outcomes, should compare the BPVP method to laser vaporization.