Researchers evaluated patients in the four-year, Phase 3 REDUCE clinical study and found that chronic prostate inflammation is associated with higher International Prostate Symptom Scores (IPSS), larger prostate volume, and acute urinary retention (AUR), but does not predict the development or progression of benign prostatic hyperplasia (BPH) with lower urinary tract symptoms (LUTS).
Further analysis uncovered that the severity of chronic inflammation was slightly associated with the development or progression of BPH/LUTS. The analysis could not confirm that acute prostate inflammation increased the incidence of development or progression of BPH/LUTS.
The study, “Chronic Prostate Inflammation is Associated with Severity and Progression of Benign Prostatic Hyperplasia, Lower Urinary Tracy Symptoms and Risk of Acute Urinary Retention,” was published in The Journal of Urology.
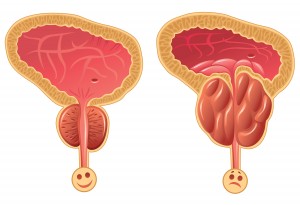 Underlying health factors driving development and progression of BPH are still largely unknown. But research proposed that inflammation of the prostate may promote BPH. For the current study, post hoc analysis of REDUCE patient data was used to determine whether inflammation correlates with BPH development and progression.
Underlying health factors driving development and progression of BPH are still largely unknown. But research proposed that inflammation of the prostate may promote BPH. For the current study, post hoc analysis of REDUCE patient data was used to determine whether inflammation correlates with BPH development and progression.
Both acute and chronic prostate inflammation were assessed by examining pre-trial patient biopsies for the presence of specific immune cells. The presence of macrophages was scored as chronic inflammation, while acute inflammation was scored simply as acute inflammation. Patients were examined every six months for four years to measure BPH symptoms such as peak urinary flow, post-void residual, IPSS, and quality of life.
IPSS, used to standardize rapid screening for BPH diagnosis, asks eight questions to evaluate symptoms such as incomplete bladder emptying, urgency, frequency, straining, nocturia, stream rate, intermittency, and quality of life which are scored on a scale from 1-5. Scores are rated from mild to severe based on the number of symptoms and degree of severity.
In the longitudinal analysis of the study, BPH development was defined as an IPSS score beyond 8. For participants who entered the study with BPH, disease progression was defined as an increase in the IPSS score of 4 points or more.
The study identified age-related associations with acute and chronic prostate inflammation, with acute inflammation more prominent in younger men, and chronic inflammation more prominent in older men.
Acute inflammation was unrelated to IPSS, and the longitudinal examination of the study found no association between acute prostate inflammation and the incidence of BPH/LUTS over the four-year trial.
Chronic prostate inflammation was associated with reduced time to risk of AUR, increased prostate size and volume, and higher IPSS.
The presence of chronic inflammation did not associate with increased incidence of BPH/LUTS development or progression. But later analysis, which used a more granular approach to evaluate the severity of chronic inflammation, showed a weak association between ‘moderate’ chronic inflammation and BPH/LUTS and suggested that the severity of chronic inflammation is associated with BPH development and progression.
Limitations to the use of the study’s longitudinal evaluation and later analysis of the REDUCE trial patient data did exist.
The REDUCE trial was designed as a cancer prevention study and to determine whether dutasteride, an oral medication used to treat BPH, would prevent prostate cancer in high risk men, so the later evaluation used only BPH data from the placebo group, which reduces the sample size for analysis.
Additionally, a larger, generalized population of men were excluded from this analysis because of the initial design of REDUCE. Finally, the extent and intensity of inflammation was not defined before the study, which complicated the use of inflammation as a measurement and potentially detracting from the statistical power in the analyses.

